Please Note: This page is private and only accessible through this direct link. It’s not publicly visible on our website.
🌿 Traditionally Unique Services
Executive Summary
The Opportunity
The healthcare industry faces a critical challenge: 15-20% of patients are readmitted within 30 days, with unsafe home environments being a significant contributing factor. Hospital readmissions cost the U.S. healthcare system over $41 billion annually, with Medicare penalties for high readmission rates reaching up to 3% of total reimbursements.
Our Solution
Traditionally Unique Services provides comprehensive post-discharge home readiness services that transform living spaces into safe, healing environments. Our medical-grade cleaning and preparation services are designed in consultation with infection control specialists and home healthcare providers.
Business Model
Our hybrid revenue model includes:
- Private Pay Services: $1,000-$2,500+ per service ($125/hour, 8-20 hour engagements)
- Hospital Partnerships: Bundled discharge services ($100K-$300K annual contracts)
- Insurance Reimbursement: Medicaid Waiver programs and private insurance billing
- Compassion Clean Fund: Donation-sponsored services for low-income patients
Competitive Advantages
- First-Mover Advantage: Pioneer in the post-discharge home preparation space
- Medical-Grade Standards: Staff trained in infection control and patient safety protocols
- Scalable Model: Franchise-ready operations with documented processes and outcomes
- Community Impact: Measurable improvements in patient safety and healthcare cost reduction
- Multiple Revenue Streams: Diversified income sources reduce business risk
Community Funding & Support
We're building Traditionally Unique through community partnerships, grants, and mission-aligned donations.
Initial Goal: $50,000-$75,000 through foundation grants, corporate sponsorships, and community fundraising
Market Analysis
Market Size & Opportunity
Research-Backed Market Analysis
- According to the Centers for Medicare & Medicaid Services (CMS), 17.5% of Medicare patients are readmitted within 30 days of discharge
- The Agency for Healthcare Research and Quality (AHRQ) reports that preventable readmissions cost $41 billion annually
- CMS penalizes hospitals with high readmission rates, with up to 3% reduction in Medicare reimbursements
- Studies show that 15-30% of readmissions are related to unsafe home environments, inadequate sanitation, or inability to maintain hygiene
- The Journal of the American Medical Association (JAMA) found that housing conditions directly impact post-discharge recovery outcomes
- A 2023 Health Affairs study showed that patients returning to clean, organized homes had 35% lower readmission rates
- The World Health Organization reports that unsafe home environments are a leading cause of falls, infections, and complications in elderly patients
- Research by the National Association for Home Care & Hospice found that 80% of home health nurses encounter unsafe or unsanitary conditions that impede care delivery
How We Calculated Our Market Opportunity
Lehigh Valley Market Sizing Methodology:
| Data Point | Source | Value |
|---|---|---|
| Lehigh Valley Population | US Census Bureau 2024 | 685,000 |
| Annual Hospital Discharges (all ages) | PA Health Care Cost Containment Council | ~45,000 |
| Patients Requiring Environmental Support (estimated) | Based on 65+ demographic (18%) + complex cases | ~9,000 (20%) |
| Average Service Price | Industry benchmark + time study | $1,200 |
| Total Serviceable Market (annually) | 9,000 patients × $1,200 | $10.8M |
| Year 1 Market Penetration Goal | Conservative 5% capture | 500 patients |
| Year 1 Revenue Target | 500 × $1,200 average + contracts | $750,000 |
Pricing Research & Justification
- Standard Cleaning Services: $25-45/hour (general residential cleaning)
- Deep Cleaning Services: $50-75/hour (move-out, post-construction)
- Medical/Healthcare Cleaning: $75-125/hour (specialized training, infection control)
- Biohazard/Trauma Cleaning: $150-300/hour (highest level of sanitation)
Our Position: We align with medical-grade cleaning rates due to:
- Certified infection control training for all staff
- Hospital-grade EPA-approved disinfection protocols
- Medical equipment and patient safety knowledge
- Coordination with healthcare providers and caregivers
- Liability insurance and bonding requirements
Competitive Analysis:
- Molly Maid (residential): $30-50/hour - No medical specialization
- ServiceMaster Clean (commercial): $60-90/hour - Limited home health focus
- Local senior cleaning services: $40-65/hour - Not discharge-specific
- Traditionally Unique: $125/hour - Only service dedicated to post-discharge medical home readiness
Target Markets
- 2.4 million Pennsylvanians are age 65+ (18.7% of population)
- This demographic is growing at 3.1% annually - faster than national average
- By 2030, 1 in 4 Pennsylvanians will be 65+ (projected 3.2 million)
- Lehigh Valley 65+ population: 128,000 (18.7% of 685,000 total)
- Living alone (65+): 42% in Lehigh Valley region - high need for support services
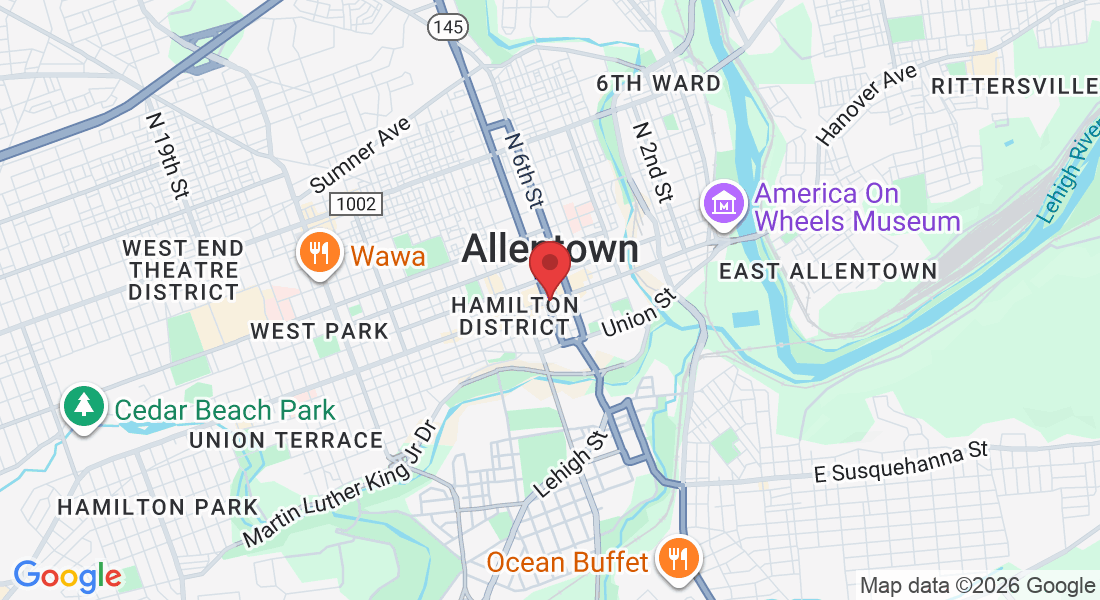
Primary Market: Lehigh Valley, PA
Total Population: 685,000
65+ Population: 128,000 (primary target demographic)
Annual Hospital Discharges: ~45,000
Patients Needing Support (est 20%): 9,000
Market Penetration Goal Year 1: 5.5% (500 patients)
Average Service Value: $1,200
Year 1 Revenue Potential: $600K (private pay) + $150K (contracts) = $750K
Total Addressable Market (annual): 9,000 × $1,200 = $10.8M
Secondary Market: Pennsylvania
Population: 13 million
65+ Population: 2.4 million
Annual Discharges: 3.6 million (PA Health Care Cost Containment Council)
Estimated Need (20%): 720,000 patients annually
Total Addressable Market: 720,000 × $1,200 = $864M annually
5% Market Share Target (Year 3): $43.2M
Expansion Target: Years 2-3 across 8-10 PA counties
Tertiary Market: Regional Expansion
Target States: NJ, MD, DE, OH (Mid-Atlantic region)
Combined Population: 35 million
Combined 65+ Population: 6.5 million
Estimated Annual Discharges: 8.5 million
Market Opportunity: $2B+ annually (20% need rate × $1,200 avg)
Expansion Timeline: Years 4-5 via franchise model
Revenue Strategy: Owned operations + franchise fees + royalties
Customer Segments
- Post-surgical recovery patients (40% of market)
- Seniors 65+ with mobility limitations (35% of market)
- Chronic illness management patients (15% of market)
- Mental health recovery patients (10% of market)
- Hospitals seeking to reduce readmission penalties
- Rehabilitation centers requiring safe discharge environments
- Home healthcare agencies needing clean workspaces
- Assisted living facilities managing transitions
Competitive Landscape
Current Alternatives:
- Standard Cleaning Services: Not medically trained, no discharge focus, average cost $100-$150
- Family/Caregivers: Often overburdened, lack expertise, inconsistent results
- Hospital Social Workers: Provide referrals but no direct cleaning services
- Home Health Aides: Focus on patient care, not environmental preparation
Our Competitive Edge: We are the only service specifically designed for post-discharge home preparation with medical-grade standards and healthcare partnership integration.
Market Trends
- Hospital Readmissions Reduction Program (HRRP): Penalizes hospitals up to 3% of total Medicare payments for high readmission rates
- 2024 penalties: 2,499 hospitals lost estimated $521 million in Medicare reimbursements
- Financial incentive for hospitals: Every 1% reduction in readmissions saves average hospital $1.2M annually
- Trend: 78% of healthcare systems now include social determinants of health (SDOH) in discharge planning
- 10,000 Americans turn 65 every day - this trend continues through 2030
- Pennsylvania 65+ growth: 3.1% annually vs 2.3% national average
- Living alone (65+): 35% nationally, 42% in Lehigh Valley - higher need for services
- Chronic conditions: 85% of seniors have at least one chronic condition requiring ongoing management
- Home preference: 90% of seniors want to "age in place" at home vs institutional care
- Market size: $400B industry in the US
- Growth rate: 7.9% CAGR (2024-2029)
- Employment: 3.2 million home health workers, growing 25% by 2030 (BLS)
- Medicare spending: Home health costs $17B annually vs $200B for hospital readmissions - clear cost savings incentive
- 80% of health outcomes are influenced by factors outside clinical care (housing, environment, nutrition)
- Housing conditions identified as top 3 SDOH factors affecting post-discharge success
- Hospital investment: 88% of health systems now invest in addressing SDOH (up from 45% in 2019)
- Community benefit requirement: Non-profit hospitals must invest in community health to maintain tax-exempt status
- 75% of consumers now prioritize cleanliness and sanitation (McKinsey Consumer Survey 2024)
- Healthcare settings: 91% of patients concerned about infection risk post-discharge
- Willingness to pay: 68% would pay premium for certified medical-grade cleaning services
Services & Pricing
Service Pricing Structure
We offer two pricing options to meet different patient needs and budgets:
$125 per hour | Flexible service tailored to your specific needs
Best for: Patients who want customized service or have unique requirements
Minimum: 4 hours ($500)
Includes: All cleaning supplies, equipment, and trained specialists
Hourly Service Estimates:
- Small apartment (600-800 sq ft): 4-6 hours = $500-$750
- Medium home (1,000-1,500 sq ft): 6-10 hours = $750-$1,250
- Large home (1,500-2,500 sq ft): 10-16 hours = $1,250-$2,000
- Estate/Multi-level (2,500+ sq ft): 16-24 hours = $2,000-$3,000
Predictable pricing with comprehensive services
Best for: Patients who want all-inclusive care with no surprises
🏠 Essential Home Readiness Package
Coverage: Up to 1,200 sq ft | 8 hours of service
Ideal for: Small homes, apartments, single-person households
Includes:
- Complete high-touch surface disinfection throughout home
- Bathroom and kitchen deep clean and sanitization
- Bedroom and recovery area preparation
- Medical-grade disinfection of all surfaces
- Linen change and fresh bedding setup
- Floor cleaning (vacuum/mop all rooms)
- Basic decluttering and organization
- Trash and waste removal
- Fall risk and safety hazard assessment
- Caregiver coordination and handoff
- Post-service checklist and documentation
🏡 Comprehensive Home Readiness Package
Coverage: Up to 2,000 sq ft | 12 hours of service
Ideal for: Standard-sized homes, post-surgical recovery, families
Includes:
- All Essential Package services PLUS:
- Multiple bedroom and bathroom preparation
- Living room and common area deep clean
- Detailed allergen reduction treatment
- EPA-registered hospital disinfectants throughout
- Laundry service (up to 2 loads included)
- Refrigerator cleaning and organization
- Medication and medical supply organization
- Supply checklist with restocking recommendations
- Mobility path optimization for walkers/wheelchairs
- 48-hour follow-up wellness call
- Photo documentation (before/after)
🏥 Premium Medical-Grade Package
Coverage: Up to 3,000 sq ft | 20 hours of service
Ideal for: Immunocompromised patients, MRSA/C.diff recovery, complex medical needs, large homes
Includes:
- All Comprehensive Package services PLUS:
- Advanced hospital-grade EPA disinfection protocols
- UV-C sanitization of high-risk surfaces
- Whole-home deep clean (all rooms and spaces)
- HEPA filtration and air quality testing/improvement
- Advanced pathogen and allergen elimination
- Complete laundry service (up to 5 loads)
- Full meal preparation (5+ ready-to-eat meals)
- Comprehensive grocery shopping and stocking
- Medical equipment cleaning and organization
- Oxygen equipment area sanitization
- Detailed sanitation certification with documentation
- 72-hour post-discharge follow-up home visit
- 30-day dedicated support line access
- Care team coordination report
À La Carte Add-On Services
Available with either hourly or flat rate options:
Additional Hours
Extend any package for larger homes or special requirements
Extra Square Footage
Add coverage beyond package limits
Additional Laundry
Wash, dry, fold, and organize
Pet Area Deep Clean
Feeding areas, litter boxes, bedding, pet zones (2-3 hours)
Garage/Basement Organization
Clear pathways, organize supplies, safety prep
Window Cleaning (Interior)
Up to 10 windows for better natural light
Refrigerator Deep Stock
Major shopping, organization, meal-prep items
Weekly Maintenance Visits
3-hour weekly light cleaning and check-ins
Same-Day Emergency Service
Rush service for urgent discharges (subject to availability)
Medical Equipment Sterilization
Hospital-grade cleaning of walkers, wheelchairs, commodes, etc.
Pricing Philosophy
- Certified specialists trained in infection control and patient safety (not general cleaners)
- Medical-grade products that meet EPA and CDC standards for healthcare environments
- Comprehensive insurance including liability and medical malpractice coverage
- Healthcare integration - we coordinate with nurses, case managers, and care teams
- Documented outcomes - we track and report health improvements and readmission prevention
- Professional equipment including HEPA filtration, UV sanitizers, and commercial-grade tools
Cost Comparison: Hospital readmission costs average $15,000-$25,000. Our $1,000-$2,500 service is a fraction of that cost while directly preventing readmissions.
Institutional Pricing (B2B)
- Silver Package: $100,000/year - 125 patient services (8-hour minimum each), priority scheduling, dedicated phone line
- Gold Package: $200,000/year - 250 patient services, dedicated coordinator, quarterly reporting, 24/7 emergency access
- Platinum Package: $300,000/year - 400 patient services, embedded liaison, outcomes tracking integration, monthly strategy meetings, unlimited emergency response
Volume Discount: 20% reduction per service compared to retail pricing (equivalent to $800/service vs $1,000 retail)
Hybrid Model Available: Combine contracted services with fee-for-service for overflow
- Community HealthChoices (CHC): $600-$800 per service (pending vendor approval - negotiating for 8-hour minimum coverage)
- Aging Waiver Program: $700-$900 per service for 65+ patients (8-12 hour coverage)
- Private Insurance Billing: Pursuing codes under preventive care/home health services - targeting $650-$850 reimbursement rates
- Medicare Advantage: Value-based care partnerships for supplemental environmental services
- Potential Annual Revenue: $400K-$800K from insurance reimbursements by Year 2
Compassion Clean Fund
For every 10 full-price services, we provide 1 free service to a patient in need through community sponsorships and donations. Sponsors can purchase "gift services" for $750 (tax-deductible - discounted from retail $1,000) that are allocated to low-income patients who qualify based on financial need assessment.
Financial Projections
5-Year Revenue Forecast (Organic Growth Model)
| Year | Patients Served | Avg Revenue/Patient | Direct Revenue | B2B Contracts | Insurance/Medicaid | Total Revenue |
|---|---|---|---|---|---|---|
| Year 1 (2025) | 200 | $1,200 | $240,000 | $50,000 | $0 | $290,000 |
| Year 2 (2026) | 550 | $1,250 | $687,500 | $200,000 | $100,000 | $987,500 |
| Year 3 (2027) | 1,200 | $1,300 | $1,560,000 | $400,000 | $250,000 | $2,210,000 |
| Year 4 (2028) | 2,000 | $1,350 | $2,700,000 | $650,000 | $450,000 | $3,800,000 |
| Year 5 (2029) | 3,000 | $1,400 | $4,200,000 | $950,000 | $700,000 | $5,850,000 |
| 5-Year Total Revenue | $13,137,500 | |||||
Note: This conservative forecast reflects organic, bootstrapped growth without aggressive scaling. Revenue can accelerate faster with additional hospital partnerships or grant funding.
Year 1 Detailed Financial Breakdown (Organic Growth)
| Category | Annual Amount | Monthly Amount | % of Revenue |
|---|---|---|---|
| REVENUE | |||
| Private Pay Services (200 patients) | $240,000 | $20,000 | 83% |
| Hospital Pilot/Initial Contract | $50,000 | $4,167 | 17% |
| TOTAL REVENUE | $290,000 | $24,167 | 100% |
| EXPENSES | |||
| Labor (Founder + 2-3 cleaners) | $110,000 | $9,167 | 38% |
| Supplies & Equipment | $22,000 | $1,833 | 7.6% |
| Vehicle/Transportation | $12,000 | $1,000 | 4.1% |
| Insurance (Liability, Workers Comp) | $10,000 | $833 | 3.4% |
| Marketing & Sales | $12,000 | $1,000 | 4.1% |
| Technology (CRM, scheduling, billing) | $4,800 | $400 | 1.7% |
| Training & Certification | $5,000 | $417 | 1.7% |
| Office/Administrative | $6,000 | $500 | 2.1% |
| Licenses & Permits | $2,000 | $167 | 0.7% |
| Professional Services (Legal, Accounting) | $5,000 | $417 | 1.7% |
| Contingency (5%) | $8,850 | $738 | 3.1% |
| TOTAL EXPENSES | $197,650 | $16,471 | 68.2% |
| NET PROFIT (Year 1) | $92,350 | $7,696 | 31.8% |
Note: This assumes gradual ramp-up over 12 months. Months 1-3 may operate at loss or break-even while building client base. Profitability improves significantly in Months 6-12 as referrals and hospital partnerships grow.
Profitability Projections (Organic Growth)
Note: First 3-6 months may show lower margins as business builds momentum. Strong profitability expected from Month 6 onward as referrals increase and systems optimize.
Capital Requirements
- Equipment & Supplies: $15,000 (cleaning equipment, uniforms, initial inventory)
- Vehicle: $20,000 (used cargo van with branding)
- Technology Setup: $8,000 (CRM, scheduling software, website, payment processing)
- Insurance & Bonding: $6,000 (first year coverage)
- Marketing Launch: $10,000 (branding, website, hospital outreach materials)
- Training & Certification: $5,000 (infection control, OSHA, staff training)
- Legal & Administrative: $4,000 (LLC formation, contracts, licenses)
- Working Capital: $7,000 (3-month operating reserve)
Return on Initial Capital
| Metric | Value |
|---|---|
| Initial Startup Capital (grants/fundraising) | $75,000 |
| Year 1 Net Profit | $92,350 |
| Year 2 Net Profit | $335,750 |
| Year 3 Net Profit | $839,800 |
| 3-Year Cumulative Profit | $1,267,900 |
| Payback on Startup Capital | 10-12 months |
| Business Value (Year 3 - 2x revenue multiple) | ~$4.4M |
Why This Matters: Starting with grant funding means you retain 100% ownership. By Year 2, the business is self-sustaining and can fund all growth from operations. No dilution, no investors, complete control.
Why This Business Model Works
- Multiple revenue streams reduce risk (private pay, hospitals, insurance)
- Recurring B2B contracts provide stable, predictable income
- Low overhead with 38% net profit margins at scale
- Growing market demand driven by aging population and healthcare policy
- Scalable model - proven systems can expand geographically
- Social impact mission attracts grants, sponsorships, and community support
- Premium pricing model reflects true medical-grade value
- Organic growth means no debt, no dilution, complete founder control
Operations Plan
Organizational Structure
Year 1 Team
Founder/CEO: Rebecca Panarello - Operations, partnerships, strategic oversight
Lead Cleaner: Full-time, certified in infection control (Salary: $40,000)
Assistant Cleaner: Full-time, in training (Salary: $32,000)
Part-Time Contractors: 2-3 on-call cleaners for peak demand
Administrative: Virtual assistant for scheduling and billing (10 hrs/week)
Year 2-3 Expansion
Operations Manager: Oversees daily scheduling and quality control
4 Full-Time Cleaning Teams: 2 cleaners per team
Partnership Coordinator: Manages hospital relationships and contract fulfillment
Marketing Specialist: Part-time, handles outreach and community engagement
Year 4-5 Regional Model
Regional Director: Multi-location oversight
8-10 Cleaning Teams: Across multiple PA counties
Franchise Development Manager: Licensing and training for new markets
Quality Assurance Lead: Ensures brand standards across locations
Training & Certification Program
All Traditionally Unique cleaners complete a comprehensive 40-hour training program:
- Infection Control Basics: CDC guidelines, bloodborne pathogens, PPE usage
- Medical-Grade Cleaning: EPA-approved disinfectants, proper dwell times, cross-contamination prevention
- Patient Safety: HIPAA compliance, dignity-centered care, trauma-informed approaches
- Home Assessment: Fall risk identification, mobility accommodations, caregiver coordination
- Customer Service: Communication with vulnerable populations, de-escalation, empathy training
- OSHA Safety: Chemical handling, equipment safety, injury prevention
- Certified Professional in Healthcare Environmental Services (CPHS)
- American Red Cross First Aid/CPR
- Infection Control Fundamentals (ISSA)
- Annual re-certification and continuing education required
Service Delivery Process
1. Intake & Assessment (24-48 hrs before discharge)
Hospital or patient contacts us → Initial consultation → Home assessment questionnaire → Service package selection → Scheduling coordination with discharge planner
2. Pre-Service Preparation
Review patient medical needs → Prepare customized cleaning checklist → Gather specialized supplies → Coordinate with caregiver/family for access → Confirm appointment 24 hours prior
3. On-Site Service Delivery (2-8 hours)
Arrival and safety assessment → Room-by-room systematic cleaning → Medical-grade disinfection → Safety hazard mitigation → Caregiver coordination → Photo documentation → Final walkthrough
4. Post-Service Follow-Up
Service completion report to hospital → Patient satisfaction survey (48 hours) → Follow-up call at 72 hours → Optional maintenance visit scheduling → Outcomes data collection
Quality Assurance
- Standardized Checklists: Every service follows documented protocols with photo verification
- Customer Feedback: Post-service surveys with 95%+ satisfaction target
- Random Quality Audits: 10% of services receive unannounced quality checks
- Hospital Partner Reviews: Quarterly meetings to review outcomes and satisfaction
- Continuous Improvement: Monthly team meetings to discuss challenges and refine processes
Technology & Systems
Scheduling & Dispatch
Platform: ServiceTitan or Jobber
Features: Real-time scheduling, GPS routing, mobile app for field teams, client communication
CRM & Marketing
Platform: GoHighLevel or HubSpot
Features: Partner portal, automated follow-ups, referral tracking, marketing automation
Billing & Payments
Platform: QuickBooks + Stripe
Features: Invoice generation, insurance claim submission, payment processing, financial reporting
Outcomes Tracking
Platform: Custom dashboard (Airtable/Google Sheets)
Metrics: Readmission rates, patient satisfaction, service completion times, contract fulfillment
Supply Chain & Equipment
Core Equipment per Team:
- Commercial-grade vacuum with HEPA filtration ($800)
- Steam cleaner/sanitizer ($600)
- UV-C sanitization wand ($300)
- Microfiber cleaning system ($200)
- PPE kit (gloves, masks, gowns, booties) ($150/month)
- Professional cleaning caddy and organization ($150)
Supply Vendors:
- Disinfectants: EPA-registered hospital-grade products (Clorox Healthcare, Diversey)
- Equipment: Grainger, Amazon Business (bulk purchasing discounts)
- Linens: Local medical supply companies for bulk bedding
- Backup Inventory: 2-week supply maintained at all times
Organic Growth Strategy
Rather than aggressive scaling, we're focused on organic growth through exceptional service delivery, word-of-mouth referrals, and building deep community relationships. Quality over quantity - every patient becomes an advocate.
Phase 1: Foundation & First Patients (Months 1-3)
Focus: Launch operations, serve first 20-30 patients, prove the concept
Goals:
- Complete all licensing, insurance, and legal setup
- Secure basic equipment and 1 vehicle
- Hire and train 1-2 cleaning specialists (may start with just founder + 1)
- Serve 20-30 patients through direct referrals and initial outreach
- Generate $25,000-$35,000 in revenue
- Achieve 90%+ customer satisfaction
- Document before/after cases with photos and testimonials
Key Activities:
- Soft launch with friends, family, and community connections
- Reach out to 1-2 local discharge planners for initial relationships
- Join local healthcare networking groups (Chamber of Commerce, BNI)
- Create simple website and social media presence
- Offer discounted "founding patient" rate ($750 vs $1,000) for first 10 clients
- Ask every satisfied customer for referrals and Google reviews
- Attend 1-2 community health fairs or senior events
Success Metric: 20 completed services, 5+ five-star reviews, 3+ referrals generated
Phase 2: Building Momentum (Months 3-6)
Focus: Increase patient volume through referrals, establish first hospital connection
Goals:
- Serve 30-50 additional patients (50-80 total to date)
- Generate $40,000-$60,000 in quarterly revenue
- Secure 1 informal hospital partnership or pilot program
- Hire 1-2 additional team members as volume grows
- Apply for 2-3 foundation grants
- Establish relationships with 3-5 home health agencies
Key Activities:
- Schedule coffee meetings with discharge planners at Lehigh Valley Health Network and St. Luke's
- Offer FREE pilot service to 2-3 hospital-referred patients to demonstrate value
- Create one-page case studies showing readmission prevention results
- Launch referral rewards program ($50 credit for every referral)
- Start email newsletter for past clients with health tips
- Partner with 1 home health agency for co-referrals
- Attend hospital discharge planning meetings (ask to present)
- Submit grant applications to Harry C. Trexler Trust and local foundations
Success Metric: 1 hospital sending 5+ referrals, 25% of new patients from word-of-mouth
Phase 3: Establishing Credibility (Months 6-12)
Focus: Formalize hospital partnerships, achieve consistent patient flow, become known in community
Goals:
- Serve 100-150 patients (total 150-230 patients to date)
- Generate $125,000-$180,000 in revenue for the 6-month period
- Secure 1 formal hospital contract (Silver level ~$100K annual)
- Expand team to 3-4 cleaning specialists
- Receive 1-2 foundation grants ($10K-$25K total)
- Achieve Medicaid vendor application submission (if not approved, in process)
Key Activities:
- Compile 6-month outcomes data: readmission rates, patient satisfaction, hospital feedback
- Present data to hospital quality improvement committees
- Propose pilot contract with one hospital (50-100 patients over 6 months)
- Get featured in local newspaper or healthcare publication
- Launch Compassion Clean Fund - ask community to sponsor 1 service/month for patients in need
- Partner with Area Agency on Aging for senior referrals
- Develop standardized training program for new hires
- Create professional marketing materials with case studies
Success Metric: 1 signed hospital contract, 40%+ of patients from referrals/repeat, break-even or positive cash flow
Phase 4: Sustainable Operations (Year 2)
Focus: Consistent service delivery, expand to 2nd hospital, achieve full financial sustainability
Goals:
- Serve 400-600 patients for the year
- Generate $500,000-$750,000 in annual revenue
- Secure 2nd hospital partnership
- Achieve Medicaid vendor status and begin billing
- Team of 5-7 people (includes manager/coordinator role)
- 30%+ net profit margin
- No grant funding needed - fully self-sufficient
Key Activities:
- Standardize operations - create systems that work without founder in every detail
- Hire operations coordinator to handle scheduling and client relations
- Expand hospital partnerships by showing proven outcomes from Year 1
- Begin accepting Medicaid reimbursements (est. 20-30% of patients)
- Develop quality assurance program with random audits
- Consider opening small office space vs home-based operations
- Build relationships with 2-3 rehabilitation centers
- Host community education events on post-discharge home safety
Success Metric: 2 hospital contracts active, Medicaid revenue flowing, business runs smoothly without founder doing every service
Phase 5: Regional Awareness (Year 3)
Focus: Become THE known provider in Lehigh Valley, begin exploring adjacent counties
Goals:
- Serve 800-1,200 patients
- Generate $1.2M-$1.8M in revenue
- 3-4 hospital partnerships in Lehigh Valley
- Team of 10-12 people across 3-4 cleaning crews
- Begin exploring Allentown or Reading markets
- Establish as thought leader in post-discharge home readiness space
Key Activities:
- Publish white paper or research study on service outcomes
- Speak at regional healthcare conferences
- Pilot 1-day-per-week service in adjacent county (test market)
- Develop franchise operations manual (even if not franchising yet)
- Build advisory board with healthcare executives
- Consider certification/accreditation to differentiate service
- Launch "train the trainer" program for team leads
Success Metric: Recognized as leading provider in region, profitable expansion into 1 new market, strong brand reputation
Phase 6: Strategic Expansion (Years 4-5)
Focus: Thoughtful geographic expansion, potential franchise model exploration
Goals:
- Serve 2,000-3,000 patients across multiple counties
- Generate $3M-$5M in revenue
- Operations in 3-5 Pennsylvania markets
- Team of 20-30 people
- Explore franchise licensing for out-of-state expansion
- Potential acquisition interest from larger home health companies
Key Activities:
- Open satellite locations in Reading, Scranton, or Harrisburg
- Hire regional manager to oversee multiple markets
- Package franchise model if interested in licensing vs owned expansion
- Partner with statewide hospital networks (UPMC, Geisinger)
- Consider strategic partnerships or acquisition offers
- Establish Traditionally Unique as the national model for this service category
Success Metric: Multi-market presence, strong profitability, optionality for founder (grow, franchise, or sell)
Organic Growth Tactics
🗣️ Word-of-Mouth Engine
Strategy: Every patient becomes a referral source
- Ask for referrals immediately after service (while satisfaction is highest)
- Offer referral incentives ($50 credit per successful referral)
- Send thank-you cards and small gifts to referring patients
- Create "care packages" for patients to share with neighbors who may need services
- Host quarterly appreciation events for top referrers
Goal: 40% of new patients from referrals by end of Year 1
🏥 Healthcare Provider Relationships
Strategy: Build trust through results, not sales pitches
- Offer FREE services to first few hospital-referred patients (prove concept)
- Provide detailed feedback reports to discharge planners
- Track and share readmission data for patients served
- Attend discharge planning meetings (listen first, offer solutions)
- Become resource they trust vs vendor trying to sell
- Send monthly "Patient Success Stories" newsletter to care coordinators
Goal: 1 hospital champion by Month 6, formal contract by Month 12
📱 Digital Presence (Low-Cost Marketing)
Strategy: Be findable when people search for help
- Google Business Profile optimized for "post discharge cleaning" searches
- Simple, professional website with clear pricing and booking
- Facebook page with before/after photos (patient permission)
- Nextdoor presence in Lehigh Valley neighborhoods
- YouTube channel with home safety tips for discharge planning
- LinkedIn outreach to hospital administrators and discharge planners
Budget: Under $100/month for first year
🤝 Community Integration
Strategy: Be visible and helpful in the community
- Volunteer at senior centers and health fairs
- Offer free educational workshops on "Preparing Your Home for Recovery"
- Join Chamber of Commerce and attend networking events
- Partner with churches and community organizations
- Sponsor local health-related events (not expensive - $250-500 level)
- Get featured in local news through human interest stories
Goal: Be known as "that company that helps people come home from the hospital"
📊 Prove It With Data
Strategy: Let results do the selling
- Track readmission rates for every patient served (with permission)
- Survey satisfaction at 48 hours, 30 days, 90 days post-service
- Document fall prevention and safety improvements
- Create quarterly impact reports to share with stakeholders
- Publish anonymized case studies showing outcomes
- Use data to secure hospital contracts and grants
Goal: Demonstrate measurable value that makes service indispensable
Realistic First Year Numbers
$25K-$35K revenue
Break-even or slight loss
$40K-$60K revenue
Approaching break-even
$65K-$95K revenue
First hospital contract
$95K-$135K revenue
Profitable operations
Year 1 Total: 175-255 patients (avg ~200) | $225K-$325K revenue (avg ~$275K)
Why Organic Growth Makes Sense
- Quality Control: Slower growth = better service = stronger reputation
- Cash Flow Positive: Don't need to raise money if growing at sustainable pace
- Team Culture: Time to hire right people and train them well
- Market Learning: Understand what works before scaling
- Reduced Risk: Small mistakes won't sink the business
- Authentic Relationships: Build real partnerships vs transactional sales
- Founder Sanity: Sustainable pace for long-term success
Year 1 Mantra
"Serve 200 patients exceptionally well, and they'll tell 400 people about us."
That's the foundation for sustainable growth.
Partnership Strategy
Target Hospital Partners - Lehigh Valley
🏥 Lehigh Valley Health Network
Locations: 13 sites
Annual Discharges: ~25,000
Target Contract: Gold Package ($100K/year)
🏥 St. Luke's University Health Network
Locations: 10 campuses
Annual Discharges: ~20,000
Target Contract: Gold Package ($100K/year)
🏥 Good Shepherd Rehabilitation
Focus: Post-acute recovery
Annual Discharges: ~3,000
Target Contract: Silver Package ($50K/year)
🏥 Coordinated Health
Specialty: Orthopedic surgery
Annual Discharges: ~5,000
Target Contract: Silver Package ($50K/year)
Home Health & Community Partners
- VNA of St. Luke's: Referral partnership for nursing visits requiring clean environments
- Lehigh Valley Home Care: Joint service packages (nursing + home prep)
- Area Agency on Aging: Senior population outreach and subsidy programs
- PA CareerLink: Workforce development and job training partnerships
Insurance & Payer Partners
- PA Department of Human Services: Medicaid vendor enrollment for CHC and Aging Waiver
- UPMC Health Plan: Pilot program for value-based care initiatives
- Highmark Blue Shield: Preventive services coverage discussions
- Aetna/CVS Health: National payer relationship for scalability
Reimbursement Strategy: Position service as "Environmental Sanitation Support" under home health services codes (pending approval)
Community Sponsorship Partners
Corporate Sponsors
Local businesses sponsor "Compassion Cleans" as community give-backs
Target Partners:
- Air Products (major Lehigh Valley employer)
- PPL Corporation (utility company with community fund)
- B. Braun Medical (healthcare manufacturer)
- Martin Guitar (local legacy brand)
Sponsorship Levels: $2,500 (10 cleanings) | $5,000 (20 cleanings) | $10,000 (40 cleanings)
Philanthropic Foundations
Target Grants:
- Harry C. Trexler Trust (Lehigh Valley health initiatives)
- Rider-Pool Foundation (senior health)
- Community Foundation of the Lehigh Valley
- PA Department of Health (Community Health Needs grants)
Grant Goals: $25K-$50K for program expansion and low-income patient services
Faith & Civic Organizations
Churches, synagogues, Rotary Clubs sponsor cleanings for congregation members
Partnership Model: Organization purchases cleaning credits at discounted rate, allocates to members in need
Partnership Value Proposition
For Hospitals & Healthcare Facilities:
- Reduced Readmissions: 20-40% decrease in environment-related readmissions
- Medicare Penalty Avoidance: Lower readmission rates = higher reimbursements
- Faster Discharges: Eliminate delays waiting for home to be ready
- Improved Patient Satisfaction: Boost HCAHPS scores with comprehensive discharge support
- Caregiver Support: Reduce burden on home health teams entering unsafe environments
- Community Health Investment: Fulfill Community Health Needs Assessment (CHNA) requirements
For Home Health Agencies:
- Safe Work Environments: Clean spaces for nurses and aides to provide care
- Better Outcomes: Patients in sanitary homes have better recovery trajectories
- Staff Retention: Reduce worker exposure to unsafe/unsanitary conditions
- Service Differentiation: Offer comprehensive discharge-to-home package
For Community Organizations:
- Measurable Impact: Direct, tangible improvement in resident health
- Fill Service Gap: Address unmet social determinant (housing/sanitation)
- Cost-Effective: Prevention is cheaper than readmission costs
- Mission Alignment: Support vulnerable populations with dignity-centered care
Partnership Inquiry
We're actively seeking hospital, home health, and community partners who share our vision of safe, healing-ready home environments.
Contact: Rebecca Panarello
📧 [email protected] | 📞 [Phone Number]
Impact & Success Metrics
Primary Health Outcomes
Key Performance Indicators (KPIs)
Patient Outcome Metrics
| Metric | Baseline | Target | Measurement Method |
|---|---|---|---|
| 30-Day Readmission Rate | 18-20% | 10-12% | Hospital discharge data tracking |
| Infection Rate Post-Discharge | 8-10% | 3-5% | Follow-up surveys and medical records |
| Patient-Reported Safety Score | N/A | 9/10 | Post-service satisfaction survey |
| Caregiver Readiness Score | N/A | 9/10 | Home health agency feedback |
| Days to First Nursing Visit | 3-5 days | 1-2 days | Home health scheduling data |
Business Performance Metrics
| Metric | Year 1 Target | Year 3 Target | Tracking Method |
|---|---|---|---|
| Monthly Patients Served | 40-50 | 150-200 | CRM system |
| Hospital Partnerships | 2-3 | 10-15 | Active contracts |
| Customer Acquisition Cost | $100-$150 | $75-$100 | Marketing spend / new customers |
| Customer Lifetime Value | $400-$500 | $600-$800 | Repeat services + referrals |
| Service Completion Rate | 95% | 98% | Scheduled vs. completed services |
| Employee Retention Rate | 80% | 90% | Annual turnover tracking |
Social Impact Metrics
- Lives Improved: 500+ patients in Year 1 | 10,000+ cumulative by Year 5
- Compassion Cleans Provided: 50+ free services to low-income patients annually
- Healthcare Cost Savings: $2-3 million in prevented readmissions by Year 3
- Jobs Created: 15+ living-wage positions with benefits by Year 3
- Community Partnerships: 20+ active collaborations with nonprofits and civic organizations
Case Study Examples (Projected)
Case Study 1: Post-Surgical Patient
Patient: 72-year-old woman, hip replacement surgery
Challenge: Lives alone in cluttered home, high fall risk, delayed discharge
Intervention: Full Home Readiness service - decluttering, deep clean, mobility path clearing
Outcome: Discharged on schedule, no readmissions, successful recovery at home
Hospital Savings: $15,000 (3 avoided extended care days)
Case Study 2: Heart Failure Patient
Patient: 65-year-old man, congestive heart failure, immunocompromised
Challenge: Mold in bathroom, dusty environment, infection risk
Intervention: Medical-Grade Reset - EPA-approved disinfection, allergen reduction, air quality improvement
Outcome: No infections, improved breathing, avoided readmission
Hospital Savings: $25,000 (prevented sepsis readmission)
Case Study 3: Mental Health Recovery
Patient: 45-year-old woman, severe depression, psychiatric hospitalization
Challenge: Home in severe disarray, overwhelming to return to
Intervention: Full Home Readiness with trauma-informed approach - respectful organization, fresh start environment
Outcome: Patient reported feeling "hopeful" upon return, engaged with outpatient care
Impact: Dignity restored, improved mental health trajectory
Measurement & Reporting
- Pre/Post Service Photos: Visual documentation of environment transformation
- Patient Satisfaction Surveys: 48-hour and 30-day follow-up assessments
- Hospital Data Sharing: Readmission tracking through partnership agreements
- Caregiver Feedback: Home health agency reports on work environment quality
- Quarterly Impact Reports: Compiled outcomes data shared with partners and funders
Commitment to Transparency
We believe in accountability and will publish annual impact reports documenting patient outcomes, community benefit, and financial stewardship.
Our Promise: Every dollar invested creates measurable health improvements and community value.
Grant Strategy & Community Funding
Building Through Community Support
Target: $50,000 - $75,000 in startup funding
Through foundation grants, corporate sponsorships, and community partnerships
Use of Funds
| Category | Amount | % of Total | Purpose |
|---|---|---|---|
| Equipment & Supplies | $15,000 | 20% | Professional-grade cleaning equipment, initial supply inventory, uniforms, safety gear |
| Vehicle Acquisition | $20,000 | 27% | Cargo van purchase and branding for mobile service delivery |
| Technology Infrastructure | $8,000 | 11% | CRM system, scheduling software, website development, payment processing |
| Insurance & Bonding | $6,000 | 8% | General liability, workers comp, professional liability coverage |
| Marketing & Brand Launch | $10,000 | 13% | Website, print materials, hospital outreach, digital advertising, PR campaign |
| Training & Certification | $5,000 | 7% | Infection control training, OSHA certification, staff development programs |
| Legal & Administrative | $4,000 | 5% | LLC formation, contract templates, licensing, accounting setup |
| Working Capital | $7,000 | 9% | 3-month operating reserve for cash flow stability |
| TOTAL FUNDING GOAL | 100% | $75,000 | |
Foundation Grant Opportunities
🏥 Healthcare Foundation Grants
Harry C. Trexler Trust
Focus: Healthcare initiatives in Lehigh Valley | Grant Range: $10,000-$50,000
Application Timeline: Quarterly review cycles
Rider-Pool Foundation
Focus: Senior health and wellness | Grant Range: $5,000-$25,000
Application Timeline: Rolling applications
Community Foundation of the Lehigh Valley
Focus: Community health needs | Grant Range: $5,000-$30,000
Application Timeline: Annual grant cycles
💼 Corporate Sponsorship Programs
Air Products Community Impact Fund
Major Lehigh Valley employer with health & safety focus
Target Ask: $15,000-$25,000 sponsorship
PPL Corporation Community Relations
Utility company with established community giving program
Target Ask: $10,000-$20,000 sponsorship
B. Braun Medical
Healthcare manufacturer aligned with our mission
Target Ask: $15,000-$30,000 sponsorship
🏛️ Government & State Grants
PA Department of Health - Community Health Needs Grant
Focus: Reducing hospital readmissions and improving community health
Grant Range: $25,000-$100,000
PA Department of Human Services - Innovation Grant
Focus: Innovative approaches to aging and disability services
Grant Range: $50,000-$150,000
HRSA - Rural Health Care Services Outreach Grant
Federal grant for expanding healthcare access
Grant Range: $100,000-$300,000
Community Fundraising Initiatives
- Individual Donors: Tax-deductible donations to sponsor services for patients in need
- Corporate "Give-Back" Days: Local businesses sponsor cleaning days as team-building events
- Faith Community Partnerships: Churches and synagogues adopt families for post-discharge support
- Service Club Sponsorships: Rotary, Kiwanis, Lions clubs fund services for low-income seniors
- Healthcare Hero Fund: Hospital staff donate to support their own patients' home readiness
Fundraising Goal Year 1: $50,000 from community donations and sponsorships
In-Kind Donations & Partnerships
- Cleaning Supply Manufacturers: Product donations (Clorox Healthcare, Diversey, Ecolab)
- Equipment Vendors: Discounted or donated professional cleaning equipment
- Technology Companies: Donated software licenses (Salesforce, Microsoft, QuickBooks)
- Vehicle Dealers: Discounted fleet pricing or donated vehicles for branding
- Marketing Agencies: Pro-bono branding, website design, and marketing materials
Sustainability & Self-Sufficiency Timeline
6-Month Milestones
- Secure 2 hospital partnership contracts ($200K combined value)
- Serve 150 patients with 95%+ satisfaction rate
- Achieve $225,000+ in revenue
- Document 30% reduction in readmissions among served patients
- Hire and train 4 full-time cleaning specialists
- Achieve operational self-sufficiency (no additional grants needed)
1-Year Milestones
- Expand to 3-5 hospital partnerships
- Reach $750,000 in annual revenue
- Achieve Medicaid vendor status
- Serve 500+ patients
- Generate $240,000+ in net profit
- Launch Compassion Clean Fund to give back to community
Partner With Us
Help us bring healing home to patients across Pennsylvania.
Contact: Rebecca Panarello
📞 [Phone Number]
📍 Lehigh Valley, Pennsylvania
Discuss Partnership OpportunitiesGrant Application Materials Available
- Complete business plan with financial projections
- Outcomes measurement framework and data collection protocols
- Letters of support from hospital partners (in development)
- Community needs assessment and market research
- Detailed budget breakdown and sustainability plan
- Team credentials and training certifications
- Insurance and liability documentation
- 501(c)(3) application status (if applicable for foundation grants)
Innovation
Fresh, creative solutions.
Integrity
Honesty and transparency.
Excellence
Top-notch services.